Diabetes may seem like an issue high school students don’t need to worry about being diagnosed with for at least a couple of decades. While the disease affects 29.1 million people in the United States, according to a 2014 Centers for Disease Control and Prevention report, the International Diabetes Federation found that the largest population of diabetics are 40 to 59 years old, more than two decades older than the typical high school senior.
But for sophomore Brooke Eckl, the disease has already become part of her everyday life in the form of Type 1 diabetes.
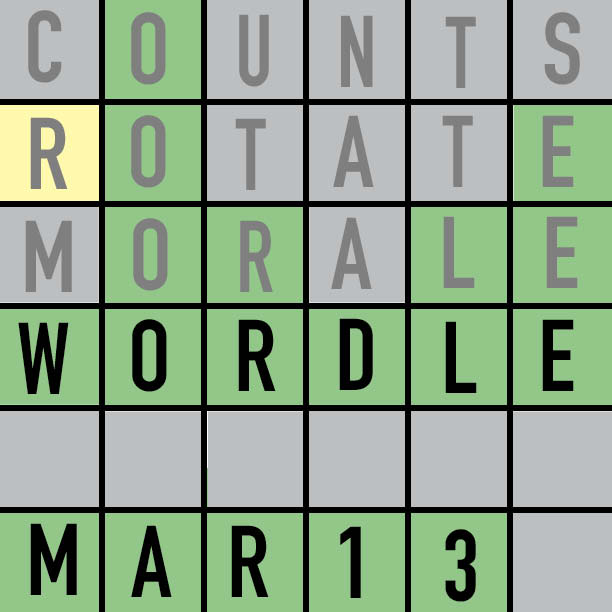
Despite awareness campaigns—November is American Diabetes Month and World Diabetes Day is tomorrow—Eckl said society still possesses deep misunderstandings about Type 1 diabetes due to its relative rarity in comparison to Type 2 diabetes.
“Type 2 is becoming a lot more common…so we’re becoming more aware of that,” she said. “But then (people) automatically stereotype you like, ‘You can’t eat sugar because you have diabetes Type 2, because you’re obese.’ And I’m like, ‘Not really. Not really.’”
Sarah Gillim, Principles of Biomedical Sciences teacher, said many people can’t tell the variants of diabetes apart.

“I think people get confused about the difference between Type 1 and Type 2. In Type 2, we know that lifestyle issues are very important (risk factors), whereas in Type 1 diabetes, the person has no personal responsibility for what happens at all. It’s the cards they were dealt. It’s (caused by) a very particular genetic makeup and perhaps something they were exposed to at one point, but they have no control over that.”
Type 1 diabetes is usually an autoimmune disorder, in which the person’s own immune cells attack beta cells in the pancreas,” she said. “Those are the cells that make insulin, so those cells get destroyed and the person’s pancreas can no longer make insulin. Type 2 is more commonly seen in adults. It’s basically a result of insulin resistance, so cells don’t respond properly to insulin.”
Type 2 diabetes is typically treated through diet, exercise and sometimes oral medications. According to Gillim, some Type 2 diabetics may need lifelong insulin infusions if beta cells “burn out” after working in overdrive to make up for insulin resistance.
On the other hand, Type 1 diabetics require insulin for the rest of their lives, as their pancreases don’t produce enough.
However, the insulin doesn’t have to come in th e form of injections.
e form of injections.
“Sometimes people will think that you always have to give shots and (use) needles,” Eckl said. “People automatically have that in their brains.”
Eckl now uses an insulin pump, but when she was first diagnosed with Type 1 diabetes at the age of 7, she injected herself with insulin after every meal. Even then, she said she felt uncomfortable in public. Others didn’t understand what she was doing.
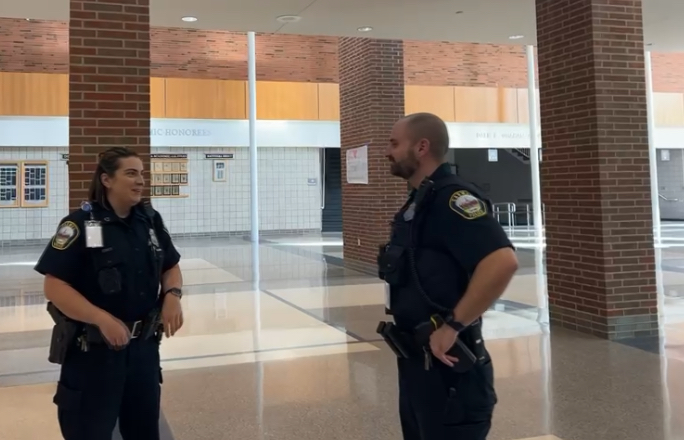
“People just stare at you. I remember I was once at Disney World and I was giving myself a shot. Some police officer came up to me and was like, ‘What are you doing?’ And I was like, ‘Um, I have diabetes,’” she said. “I felt really awkward just sitting there with my dad. Doing it in public was kind of weird; I’d rather do it at my house or do it in a bathroom.”
She said switching to a pump, a pager-sized device that directly infuses preloaded insulin into the body through changeable plastic tubing, allowed for greater convenience and privacy. Now, she keeps track of all the carbohydrates she eats and programs the pump to provide the correct amount of insulin to keep her blood sugar regulated.
According to the American Diabetes Association (ADA), insulin pumps supply “basal” insulin continuously and add “bolus” amounts for mealtimes, when blood sugar levels increase.
Even though using the pump is more discrete than injecting herself, Eckl said many people will still misinterpret what the pump is for.
“I wear my pump on my side, so people will always stare at it,” she said. “It’s kind of funny because they’re always looking at it weirdly, and I’m like, ‘Nope, it’s okay.’ I get really weird comments like, ‘Is that a wallet?’ because I used to wear a little pouch. (People would ask me,) ‘Is that a pedometer? Is that a pacemaker?’”

Like Eckl, all registered diabetics at CHS have Type 1, according to school nurses Rachel Basey and Julie Beihold.
Basey said most of them self-manage using insulin pumps. As a result, the health center now sees fewer diabetic students for insulin-related reasons.
But even though CHS’s diabetics visit the nurse infrequently, improperly managing blood sugar can still be potentially life-threatening.
“If I don’t give myself enough insulin, I can run high, which then is not good because my body has too much sugar, and I start feeling really sick. I get really thirsty or get a really weak feeling,” Eckl said. “A lot of people have (diabetes), so (others are) like, ‘Oh, it’s not that bad.’ But it could kill you if you don’t care of it. If your blood sugar gets too high or too low, you could go into a coma. That’s very scary. There’s a thin line between being regulated or not.”
Basey said having diabetes puts patients at risk for a host of complications in the future.
“In the long term, you can lose extremities (and) digits. You can impact your kidneys. You can have a loose sensation in your fingers and your toes, and it makes you more prone to injuries you don’t feel.”
If your blood sugar gets really low, you can have a seizure and go unconscious, in which case someone else would have to treat you with sugar. That could be life-threatening if you were by yourself,” Basey said. “And if you get really high (on glucose) and don’t manage your symptoms, you could have something called D.K.A., diabetic ketoacidosis, that you usually have to be hospitalized (for in order) to get your blood sugar down. If it goes untreated it can cause swelling in your brain.”
According to Mayo Clinic, diabetics have an increased risk of cataracts and blindness resulting from retinopathy, a condition in which the eye grows poorly formed blood vessels to replace blocked ones.
On the brighter side, carefully controlling blood sugar dramatically decreases the risks of a complication.
But aside from monitoring glucose levels, there is also an emotional side to being diagnosed with diabetes.
“My Type 1 just came out of the blue…as a kid, I was very scared when I first got diagnosed,” Eckl said. “I was a needle-phobic. I was so scared of needles. I remember one time when I was 4 years old, I had to get my blood drawn…I kept running around the room saying, ‘I don’t want to do this.’ Four of the nurses had to hold me down to get a shot, so (when she found out I had Type 1), my mom was like, ‘No. Not her. She can’t have this.’”
Type 1 diabetes has also been linked to Celiac disease, another autoimmune disorder characterized by gluten intolerance. Eckl has the disease and as a result cannot consume gluten.  However, she said some people think diabetics have to avoid all carbohydrates—an obviously untrue statement because some diabetics need a readily available source of sugar in case of low blood glucose, according to Gillim.
However, she said some people think diabetics have to avoid all carbohydrates—an obviously untrue statement because some diabetics need a readily available source of sugar in case of low blood glucose, according to Gillim.
“Usually (people are) like, ‘You can’t eat sugar,’ or like, ‘You can’t eat certain foods,’” Eckl said. However, according to her, there actually isn’t an upper limit to how much sugar she can
eat—the catch is, she has to read the Nutrition Facts label, count the carbohydrates and plug the numbers into her pump. But even without a ceiling for carbohydrate consumption, she said she doesn’t go overboard with the sugar.
“I probably could have five cans of soda…when I first got diagnosed, the doctor was telling (my mom), ‘Oh, nope, (your daughter’s) fine. She can have as much sugar as she wants,’” Eckl said.
“Certain people have different limits. Certain diabetics can only have 200 carbs a day or 15 carbs a meal, but mine’s more free reign, where I can do whatever I want and just watch my limits. I had to make it a part of my lifestyle…I have to stay healthy. When we were little, a lot of my friends were eating a bunch of candy and cake. I kind of felt left out,” Eckl said. “I could eat those things, but I had to give myself a shot for it. Doing that out in public is kind of embarrassing. I had to limit myself on some of those things, which was a little unusual.”
Even though diabetics must be more aware of how they feel and what they eat, Basey said having diabetes doesn’t impose any large limits on them.
“People are surprised when (Type 1 diabetics are) athletes, or when they’re in a lot of activities that require a lot of physical action,” she said. “The diabetes doesn’t keep them from doing anything. It may just require adjusting how they manage. If you were going to run a marathon, you would just have to be more cognizant of food and your blood sugar than a (non-diabetic) person.”
Eckl now participates in marching band. She also played soccer in elementary and middle school. According to her, being an athlete simply meant modifying her schedule.
“I would just adapt how I acted,” she said. “I had to eat food for my games so my blood sugar wouldn’t drop low. I had to make different acc ommodations.”
ommodations.”
In fact, Gillim said making lifestyle changes in order to manage Type 1 diabetes can even make students more responsible.
“It’s kind of shocking for the kid to have to deal with (diabetes), but I’ve known plenty of students that handle it very well,” she said. “In some ways, I think (diabetes is) something they learn to handle, and that’s a type of responsibility that other kids don’t have to face, so it matures them a little more quickly than other kids their age.”
Even though many misconceptions persist about the disease, especially its Type 1 variant, Eckl said the situation is improving through teaching students about diabetes in science and health classes and donating to organizations such as the Juvenile Diabetes Research Foundation and the ADA in hopes of finding a cure.
“I feel like (people would stop staring if they were more educated). (Diabetes) is more common (now). More people are more aware of it,” she said. “But before, people, especially younger people, would look at me weirdly, like, ‘What are you doing?’”
Most of all, Eckl emphasized people shouldn’t jump to conclusions.
“A lot of people, when I first meet them, have a stereotype in their mind about how diabetics are. But then once they get to know me, they realize that I’m not much different (from them),” she said. “Research it. Know about it before you make the judgment. Don’t judge a book by its cover. Even though I say I have diabetes, there’s a deeper meaning to it. It’s not just about blood sugar. It’s part of who I am.”
























![AI in films like "The Brutalist" is convenient, but shouldn’t take priority [opinion]](https://hilite.org/wp-content/uploads/2025/02/catherine-cover-1200x471.jpg)

















![Review: “The Immortal Soul Salvage Yard:” A criminally underrated poetry collection [MUSE]](https://hilite.org/wp-content/uploads/2025/03/71cju6TvqmL._AC_UF10001000_QL80_.jpg)
![Review: "Dog Man" is Unapologetically Chaotic [MUSE]](https://hilite.org/wp-content/uploads/2025/03/dogman-1200x700.jpg)
![Review: "Ne Zha 2": The WeChat family reunion I didn’t know I needed [MUSE]](https://hilite.org/wp-content/uploads/2025/03/unnamed-4.png)
![Review in Print: Maripaz Villar brings a delightfully unique style to the world of WEBTOON [MUSE]](https://hilite.org/wp-content/uploads/2023/12/maripazcover-1200x960.jpg)
![Review: “The Sword of Kaigen” is a masterpiece [MUSE]](https://hilite.org/wp-content/uploads/2023/11/Screenshot-2023-11-26-201051.png)
![Review: Gateron Oil Kings, great linear switches, okay price [MUSE]](https://hilite.org/wp-content/uploads/2023/11/Screenshot-2023-11-26-200553.png)
![Review: “A Haunting in Venice” is a significant improvement from other Agatha Christie adaptations [MUSE]](https://hilite.org/wp-content/uploads/2023/11/e7ee2938a6d422669771bce6d8088521.jpg)
![Review: A Thanksgiving story from elementary school, still just as interesting [MUSE]](https://hilite.org/wp-content/uploads/2023/11/Screenshot-2023-11-26-195514-987x1200.png)
![Review: "When I Fly Towards You", cute, uplifting youth drama [MUSE]](https://hilite.org/wp-content/uploads/2023/09/When-I-Fly-Towards-You-Chinese-drama.png)
![Postcards from Muse: Hawaii Travel Diary [MUSE]](https://hilite.org/wp-content/uploads/2023/09/My-project-1-1200x1200.jpg)
![Review: "Ladybug & Cat Noir: The Movie," departure from original show [MUSE]](https://hilite.org/wp-content/uploads/2023/09/Ladybug__Cat_Noir_-_The_Movie_poster.jpg)
![Review in Print: "Hidden Love" is the cute, uplifting drama everyone needs [MUSE]](https://hilite.org/wp-content/uploads/2023/09/hiddenlovecover-e1693597208225-1030x1200.png)
![Review in Print: "Heartstopper" is the heartwarming queer romance we all need [MUSE]](https://hilite.org/wp-content/uploads/2023/08/museheartstoppercover-1200x654.png)